PDA – Pain, Depression, Anxiety
Low back pain (LBP) is a global issue with a prevalence point of around 8% of the world population (~ 577.0 million people). Approximately 60% of patients with chronic pain suffer, in addition, from two or more psychological conditions like depression and anxiety. In nearly 52% of the cases, LBP patients also suffer from anxiety, depression, underdiagnosed, perpetuating the economic burden and the mental conditions.
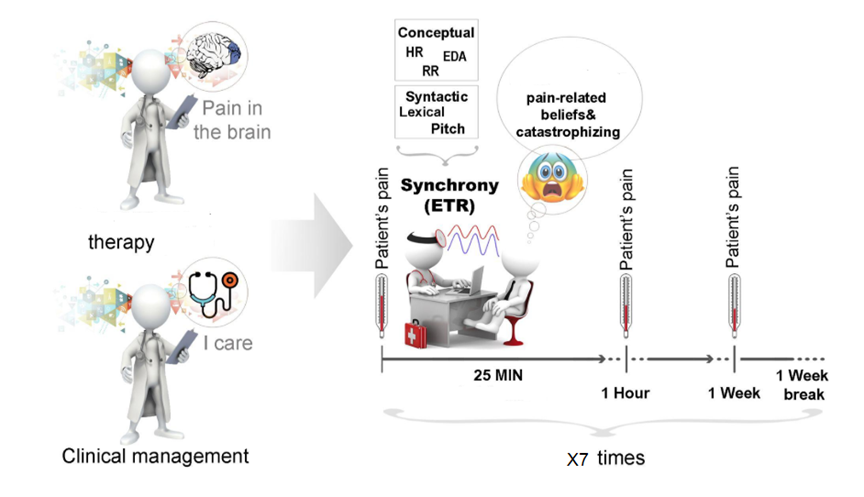
Importantly, this synergy between pain and mental health conditions may change dynamically and not be well-understood. We are focusing on researching pain, depression and anxiety that usually change over time in daily life. We build an integrative system that will combine daily self-reported assessments, physiological and behavioral digital markers.
This Also, advanced computational approaches will be used for analysis of linguistic characteristics and behavioral markers of daily life activities over time, along with physiological measures, traced by the Fitbit smart watch device.
Better understanding of the compound mechanism that underlie chronic pain and mental health conditions will allow us to improve clinical approaches and prevent aggravation of these synergetic conditions.
The study is in collaboration with, Prof. Hagit Hel-Or (Department of Computer Science), Prof. Hadas Okon-Singer (Department of Psychology, Cognition Emotion Interaction Lab), Prof. Sigal Zilcha-Mano (Department of Psychology, Psychotherapy Research Lab) and Prof. Tzvi Reiss (Department of Statistics).